PBGH Launches its Advanced Primary Care-Driven Health Care Network in Puget Sound, Washington
December 10th, 2024
Boeing, eBay and Other Large Employers Now Offering Advanced Primary Care and High-Value Specialist Referrals to Employees and Families
Purchaser Business Group on Health (PBGH), a nonprofit coalition representing 40 private employers and public entities across the U.S., today announced that the Puget Sound region of Washington is the first to offer PBGH’s Advanced Primary Care-driven health care network to eligible member employees and families. The network is a ‘system of excellence’ driven by the rigorous quality and patient care standards of PBGH’s Advanced Primary Care (APC) program and includes high-value specialty referrals to deliver comprehensive, whole person care.
Multiple PBGH employers are participating, including The Boeing Company and eBay whose combined tens of thousands of eligible employees can now access this innovative network of advanced primary care and high-quality specialists through their employer-sponsored health benefits.
“PBGH has a 35-year history of supporting employers to get the best care for their employees. We know that primary care lowers health care costs by as much as 33%, while significantly improving the health and well-being of those who regularly see a primary care provider,” said PBGH President and CEO Elizabeth Mitchell. “We are proud to partner with Boeing, eBay and other PBGH member organizations committed to better access and health outcomes at lower costs to patients. PBGH members are pleased to partner with top-quality primary care providers across the Puget Sound area to improve the health and wellbeing of their workforce.”
“PBGH identifies top providers who meet quality standards based off of clinical best practices, purchaser expectations of patient experience, and administrative transparency to achieve the PBGH Care Excellence designation,” said Raymond Tsai, M.D., MS, a Family Medicine physician serving as PBGH’s Vice President of Advanced Primary Care.
EmsanaCare, a company co-founded by PBGH, directly contracts with those providers and enables care navigation among them. Eligible employees and families gain access to a vetted network of high-quality primary care and specialty providers, and navigation services for referrals.
“By directly contracting with top primary care and specialty providers, thousands of employees and their dependents can access primary care that meets PBGH’s quality standards. By ensuring seamless navigation between primary care and top specialists , we make getting to the best care easy. Employees have improved access, satisfaction, and outcomes,” said Dane Guarino, CEO of EmsanaCare. “At the same time, employers enjoy simplified plan implementation and peace of mind that they are creating a pathway to improved health that is easier for their employees to use.”
“Our purpose is rooted in connecting people and building communities to create economic opportunity for all,” explained Rob Paczkowski, Senior Director, Global Benefits, eBay Inc. “Providing comprehensive and innovative benefits that support the health and wellbeing of our teams is vital to nurturing a culture that enables us to achieve our purpose. PBGH simplifies some of the most challenging aspects of selecting and contracting with high quality health care providers. By partnering with other employers through PBGH it makes it possible for us – in areas like Puget Sound where we have a smaller employee headcount – to provide our local teams and families with health care the way it should be delivered.”
The Puget Sound region of Washington is the first of many markets nationwide. There is currently another open request for proposal for APC providers who want to work with employers in the San Antonio, Texas market, with additional markets being planned for 2025.
###
About Purchaser Business Group on Health
PBGH is a nonprofit coalition representing nearly 40 private employers and public entities across the U.S. that collectively spend $350 billion annually purchasing healthcare services for more than 21 million Americans and their families. In partnership with its members, PBGH initiatives are designed to test innovative operational programs and scale successful approaches that lower healthcare costs and increase quality across the U.S. The PBGH System of Excellence streamlines the selection, contracting, and administration of high-quality advanced primary care, ensuring equitable and evidence-based care while flattening trend.
About EmsanaCare
EmsanaCare, co-founded by the Purchaser Business Group on Health, simplifies the adoption of advanced primary care (APC) for employers and purchasers. The solution focuses on streamlined contracting, comprehensive administrative support, and informed referrals, allowing purchasers to access multiple APC sites with a single contract. By connecting advanced primary care practices with high-value specialists and regional centers of excellence, EmsanaCare is dedicated to delivering value-driven, efficient, and high-quality primary care solutions for employers and their members.
Better Data Collection Essential to Understanding and Addressing Health Inequities
December 14th, 2022
The COVID-19 pandemic exposed and exacerbated the weaknesses of the U.S. health care system and highlighted long-standing inequities for minority communities. Highlighted during this period was the profound impact of economic stability, education, social and community life, one’s neighborhood and access to high-quality health care—social determinants of health—on the overall health and well-being of communities.
As a result, addressing health inequities has become a top priority for many employers, purchasers and health care providers. The ability to effectively collect a range of data points about patients and the care they receive is an essential component to creating meaningful change and ensuring populations achieve their full health potential.
Looking at health quality data by race, ethnicity, language and other patient characteristics, is crucial for understanding how long-standing systems of privilege and oppression impact the health of minority populations and communities. However, patient self-reported race, ethnicity and language (REaL) data across health insurance markets is widely variable and overall limited. While race and ethnicity data in California’s Medicaid program (called Medi-Cal) is broadly available likely because of legislation requiring health plans to collect this information starting in 2009, corresponding data for the majority of patients who receive health benefits through the commercial market – via employers or on the private market –is low or absent.
These limitations of known race and ethnicity data hinder the ability to see where disparities exist and for the health system to react with meaningful interventions. For health plans and large employers and purchasers, who provide health benefits for more than half the U.S., it is crucial to uncover variation in the access to care and the quality and experience of care being provided.
With better self-reported patient demographic information, employers, purchasers, payers and providers can tie this data to health care access, quality, patient experience and outcomes to illuminate exactly where disparities exist. These insights can enable tailored interventions and support for improvement.
How to Improve Data Collection
Legislation, Policy and Regulation
Legislation and regulations can incentivize or require health plans, providers and other health system organizations to increase the collection and quality of self-reported demographic data. Legislation and statute also have the potential to enforce standardization for data fields and definitions, which enables largescale purchasers of health care to align with their health plan and provider industry partners and enhance their ability to share, aggregate or disaggregate data to identify trends and implement plans for improvement.
It is crucial to ensure that national and state standards do not contradict each other.
Contracting and Business Relationships
Contracting requirements and incentives as part of large-scale public and private purchaser and payer programs can increase the collection, reporting and use of REaL data and thereby bolster efforts to mitigate disparities. Large purchasers could add incentive payouts if plans are able to stratify measures across self-reported REaL data. Health plans, provider organizations and other payers that contract within the health system can use incentive payouts for better data collection and stratification and other efforts to reduce disparities. Another approach is to build tiered networks that point patients to providers who have proven to be stronger at collecting, reporting and using REaL data.
It is important for purchasers and payers to avoid siloed initiatives that conflict with each other.
Organizational Leadership, Systems Structure and Culture
Organizations that pay for services at the point of care (e.g., health plans and independent physician associations, or IPAs) have the potential to increase REaL data collection, reporting and use by assessing and enhancing data collection opportunities, sharing data internally and creating a culture that values the collection of this information. This starts with organizational leadership. It is important to normalize data collection into regular workflows to improve the quality and ensure the most accurate information possible.
Purchasers, health plans and provider organizations can increase patient self-reporting by increasing awareness of how the data will be used and educating enrollment counselors and other staff with direct patient interaction on why it is important to collect this data.
Certification Requirements
The National Committee for Quality Assurance (NCQA) has required plans to report their percentage of self-reported REaL data for certain key measures, with a goal of 80% self-reported data. Additional accrediting organizations, purchasers and others could adopt similar certification requirements to support reporting and stratification for the same measures and self-reported data goals as NCQA. This would increase the consequences for not aligning and support the overall goal of greater availability of self-reported REaL data.
Read more in our latest issue brief.
5 Lessons for Achieving High-Quality Virtual Care
October 21st, 2022
A new report presents five lessons to support the long-term use of telehealth services as a tool to deliver high-quality virtual care.
The use of telehealth services to support patient care has rapidly expanded due to the global COVID-19 pandemic. The volume of care provided virtually jumped drastically from approximately 2% prior to the pandemic to highs of 50% or more as the initial wave of COVID-19 swept the United States.
In response, PBGH’s California Quality Collaborative launched the CalHIVE Network, an improvement collaborative focused on maximizing the use of virtual care tools to enhance chronic disease management. Over two years, the seven participating provider organizations adopted and refined telehealth strategies to improve virtual care for more than 715,000 Californians. The lessons presented here are supported by the real-world experiences of providers who participated in the CalHIVE Network.
1. Invest in people and technology
There is not a single telehealth strategy that health care organizations should adopt. Instead, they should examine their overall strategic plan, patients’ clinical needs and projected environment and decide how telehealth can be an integrated part of the overall clinical experience. This requires targeted resource investments.
Desert Oasis Healthcare, a CalHIVE participant, discovered that the shift to telehealth did not equally serve all members of its community, and even created new barriers for some. A mobile health unit was used to expand access to care. The unit provides access to a care team on-site in the mobile unit, or if preferred, patients can speak directly to their physician via the unit’s virtual exam room.
2. Support seamless data exchange and integrated clinical systems
Technology should support a seamless experience for care teams and patients, but this is often not the case because of poor integration into other clinical systems and the overall care experience. One CalHIVE participating organization surveyed network providers and found more than thirty different telehealth platforms were being used across twelve Independent Physician Associations (IPA).
Provider organizations should consider how a virtual care platform integrates with the current technology used by most of their network’s providers and ensure they understand which products are being used in their networks. Organizations may consider peer groups or information and resource sharing based on the most utilized platforms.
Many telehealth technologies are focused on primary care, rather than specialty care. This creates a huge gap when aiming for care integration. Technology and associated resources should be tailored to support as many specialties as possible.
3. Redesign clinical workflows to support telehealth
Effective team-based care has been a key attribute of high-performing primary care delivery for many years. However, when it comes to telehealth, many organizations have not had the bandwidth to redesign their workflows or may not even be sure what needs to be redesigned.
Choice Medical Group used their morning huddles to gather feedback on virtual appointment workflows and to proactively engage staff in problem solving. That feedback supported improvements to training and adjustments to their telehealth platform and workflows.
4. Collect and integrate patient and care team feedback
Understanding how your providers are using telehealth is crucial to achieving high-value virtual care. Organizations should regularly ask providers, care teams and employees about their telehealth experience to determine if workflows, training and functionality can be improved.
In a networkwide survey, PrimeCare found that the majority of its providers were offering telehealth services but were struggling with challenges related to coding, reimbursement and patient education. By using the feedback collected, the organization was able to take action to improve the quality of their virtual care visits, which led to 80% of patients reporting a positive telehealth experience. Efforts to respond to the challenges identified included implementing several centralized support services for its network by developing telehealth best practice guides, educating providers and staff through individualized meetings and adding specific telehealth-focused questions to its annual provider survey.
5. Utilize data to address known health disparities associated with virtual services
To better understand if telehealth is meeting patients’ needs, health care organizations should examine utilization, access, experience and outcomes data by key patient demographic fields to identify improvement actions needed to ensure telehealth is effective for all patients.
In trying to understand why telehealth services were being used less by their non-English speaking patients, Golden Valley Health Centers discovered that their translation service was causing poor audio quality for non-English speaking patients using video visits. Updated workflows, including a new standard work around for the “language line” instructions, and additional training and education for frontline staff have been successful in supporting non-English speaking patients.
More information about each of these lessons and the experiences of CalHIVE participants can be found here. As health care organizations prepare for the future of telehealth, these learnings can inform their decision making and offer a road map to high-quality virtual care. They may also provide insights to other stakeholders, such as purchasers, health plans, technical assistance organizations and policy makers, as they seek to support telehealth moving forward.
Strengthening Primary Care: A Pilot with Four Large Purchasers
June 10th, 2022
Extensive research and pilot programs have shown that easily accessible, person-centered and team-based primary care that integrates behavioral health and other supports can significantly improve patient outcomes and experience. It can also increase population health, reduce overall costs and serve to improve equity in our health care system.
It is for these reasons that PBGH’s California Quality Collaborative (CQC) has been working for over a decade to improve primary care. That work has culminated in the development of shared attributes and measures that enable purchasers, health plans and providers to identify primary care practices in a given market that are delivering the kind of care research tells us will bring about the best results for patients.
Together with the Integrated Healthcare Association (IHA), PBGH brought together four large health care purchasers in California to pilot this set of performance measures that emphasize patient experience and outcomes. The PBGH/IHA partnership, known as the Advanced Primary Care Measurement Pilot, began in January 2022, and participating purchasers include Covered California, California Public Employees’ Retirement System (CalPERS), eBay and San Francisco Health Services System.
Partnering to Better Primary Care in California
Our already weak primary care system has been further hampered by the pandemic, and these purchasers recognize that the time to strengthen it is now. The four participating purchasers have aligned by incorporating the same Advanced Primary Care attributes and measures into their health plan contracts. The goal is to identify the primary care practices throughout the state performing at the highest levels and delivering high-quality patient care.
The set of performance measures being tested through the pilot reflect the shared standard of Advanced Primary Care as defined through a multi-stakeholder process led by PBGH’s California Quality Collaborative that included input from purchasers, health plans, providers and patients.
The outcome will be an increase in understanding of where patients are getting the highest quality primary care. The pilot will give purchasers and health plans information to help them make decisions about their provider networks, resource distribution and consumer incentives. This information can be used to better connect patients to practices delivering Advanced Primary Care and incentivize improvement for other providers, increasing the availability of Advanced Primary Care.
How the Pilot Works: Existing Data for a New Purpose
Data already available through IHA is being used, so health plans and providers do not have to report anything new. The existing data will be used for a new purpose – to assess individual practices.
Performance information can be diluted when data from multiple practices is combined. By looking at each individual practice separately, we can gain the best understanding of which practices are delivering the best primary care and which ones need improvement.
The data will also be aggregated across purchasers and health plans for the first time to provide a more complete view of each individual practice’s performance, rather than looking at small segments of patients in a vacuum. This will allow for a better assessment of whether a practice has the systems in place to consistently provide high-quality care for everyone
Currently, ways to account for socio-economic and demographic differences in the performance analysis is being explored. This lens is crucial to ensure decisions made around the pilot promote equity and do not inadvertently increase the challenges vulnerable communities already experience in accessing high-quality care.
The analysis will include data from January through December 2022, and results and findings are expected mid-2023.
Supporting Non-Hospital Birthing Options: Employer Strategies to Improve Quality
May 23rd, 2022
Maternal infant health outcomes in the U.S. remain the worst among high-income countries, and Black women in the U.S. are nearly three times more likely to die from pregnancy-related complications than white women are. Additionally, U.S. women of reproductive age are significantly more likely to have problems paying their medical bills or to skip or delay needed care because of costs.
To underscore the high costs disproportionate to the poor maternal health outcomes, the cost of maternity care represents American employers’ second-highest annual health care expenditure – $1 in every $5. Faced with unacceptable results, employers are looking for pathways to improve maternal health care quality, affordability and the overall patient experience.
Improving Quality and Lowering Costs
Consumer surveys have shown that more patients are seeking non-hospital, community-based childbirth options, such as midwives, doulas and birth centers. This is particularly true for birth participants of color who are looking for alternatives to the hospital-physician childbirth experience.
Recent CDC 2020 vital statistics data mirror what we have seen from consumer surveys. Although overall births declined, in 2020 the number of births in birth centers nearly doubled. This is a significant indication that more women want choice in their maternity care team and care location and that more families, when given a choice, are seeking a non-hospital childbirth option.
Non-hospital maternity care options can help to address the problem of high-cost, low-quality care. Evidence shows the use of midwives improves overall maternal and infant health and decreases the cost of maternity care. In fact, research shows that collaborative care led by certified nurse midwives can result in 22% fewer primary C-sections. It also helps address a growing shortage of perinatal health providers. Despite these benefits, however, certified nurse-midwives are vastly underutilized, delivering only 9% of babies nationally.
A birth center is a midwife-led childbirth facility that offers individuals and families a more natural, lower intervention and less medicalized childbirth experience. Birth centers are freestanding facilities and separate from acute obstetric or newborn care where care is provided in the midwifery and wellness model of care. Birth centers typically have relationships with other community health providers and arrangements with other facilities, such as hospitals, for transfers to other levels of care when needed.
The CMS Strong Start program demonstrated that women who received prenatal care in birth centers had better outcomes and lower costs. This included lower rates of:
- Preterm births
- Low birth weight
- C-sections
Additionally, costs were more than $2,000 lower per mother-infant pair during birth and the following year for women who received prenatal care in birth centers.
How Purchasers Can Support Non-Hospital Options
Employers know that improving maternal health outcomes in the U.S. and reducing disparities will require changes to the existing system of care to make it more patient centered. Here are three ways employers can influence the health system and health plan leaders’ perspectives to address the barriers preventing birth center expansion, collaboration between hospitals and birth centers and access to midwives:
- Benefit design: Benefits programs can be designed to expand access to midwives and birth centers. For example, eBay has started covering out-of-network midwives at in-network rates to improve access to community providers.
- Payment and contracting: By paying for care differently and moving towards value-based payment rather than fee-for-service models, employers can greatly improve access to high-value facilities such as birth centers. A simple birth center bundled payment model would allow all prenatal, labor and delivery and postpartum care provided by the birth center to be captured under one claim/invoice. A bundled payment project with Qualcomm produced valuable lessons learned that could benefit other employers pursuing a bundled payment option.
- Quality improvement: In the event of a transfer from a birth center to a hospital, the transfer process is smooth and respectful for the patient and their family. PBGH is leading a project in California to establish a model to inform procedures regarding transfers.
In response to the lack of comprehensive, coordinated care and the overmedicalization of childbirth PBGH has developed several strategies to help employers impact their maternity marketplace.
How Primary Care Providers Can Improve Depression Screening
May 4th, 2021
Depression screening is an essential tool for primary care providers to better understand and meet their patients’ needs, especially as behavioral health conditions have dramatically increased in the past year. Patient-centric approaches and thoughtful implementation of depression screening can lead to earlier intervention, improved overall health outcomes and reduced utilization of health care services.
In March 2021, PBGH’s California Quality Collaborative (CQC) hosted a webinar on the importance of depression screening for patients, providers and payers and shared practical advice for patient-centered depression screening. Experts from PBGH, Montefiore Medical Center and UCLA identified four key takeaways during the discussion:
1. Primary care providers should start screening patients for depression now. There is increasing demand being placed on primary care clinicians to screen patients for depression. Health plans, employers and other purchasers of health care recognize that depression affects millions of patients, and they are investing in behavioral health as a strategy to improve health outcomes. In California, there is momentum from organizations like the Integrated Healthcare Association, which runs statewide performance improvement programs, and Covered California, to include depression screening as a required health care quality measure. Providers will be financially accountable for completing depression screening in the next several years as part of existing pay-for-performance programs.
2. Care teams need training to be comfortable screening patients for depression. Care teams require resources and information about depression screening and how to follow up appropriately with patients in need of behavioral health services. Specialized trainings with role-playing opportunities are effective, as are resources, such as a list of frequently asked questions developed by the Advancing Integrated Mental Health Solution (AIMS) Center from University of Washington.
3. Screening workflows can be integrated into virtual visits, with intentional planning. During the public health emergency, UCLA Health increased the use of virtual primary care visits. The system’s clinical and operations teams created a depression screening workflow that leveraged “virtual rooming” steps, during which clinical support staff register and prepare patients for telehealth visits just as they would for in-person clinical appointments. To address safety concerns associated with suicidal ideation documented in patient depression questionnaires, they tested and implemented several solutions by which the provider would monitor a patient’s response, or the electronic health record would issue an automatic alert.
4. Technology can expand the reach of primary care to provide whole-person care. Montefiore Medical Center launched a smartphone app that includes screening, educational resources, appointment and medication reminders and near real-time chat, among other features. Providers using the Montefiore app with their patients found that it improved behavioral health care engagement with a diverse set of patient populations. In an analysis of the smartphone app pilot data, 72% of patients used it to access educational articles and videos, 69% used it to interact with their care teams via secure chat or text and 67% used the app to complete a depression or other behavioral screening scale.
For additional insights about how primary care providers can improve depression screening for their patients, watch the March 31 CQC webinar or access the presentation.
The Current State of Mental Health Screening and Access in California: Results from 35,000 Patients
October 26th, 2020
Mental health concerns are increasingly common, yet many patients in California are not screened for symptoms and are unable to access treatment. Understanding patients’ access to care is challenging; data are scarce and usually only available at a statewide level, even though there are likely wide regional differences due to workforce shortages.
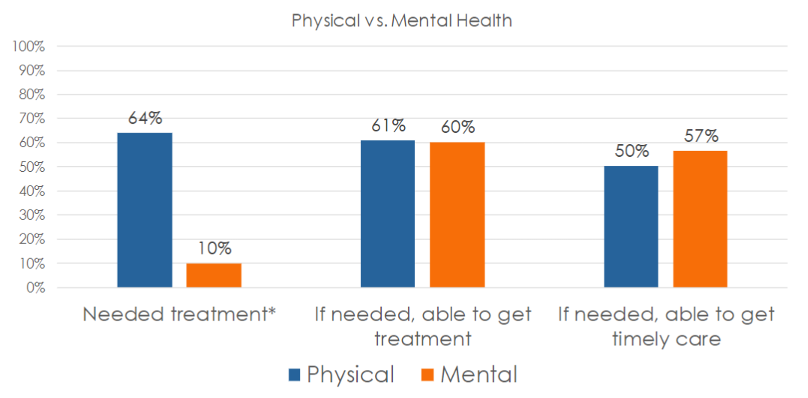
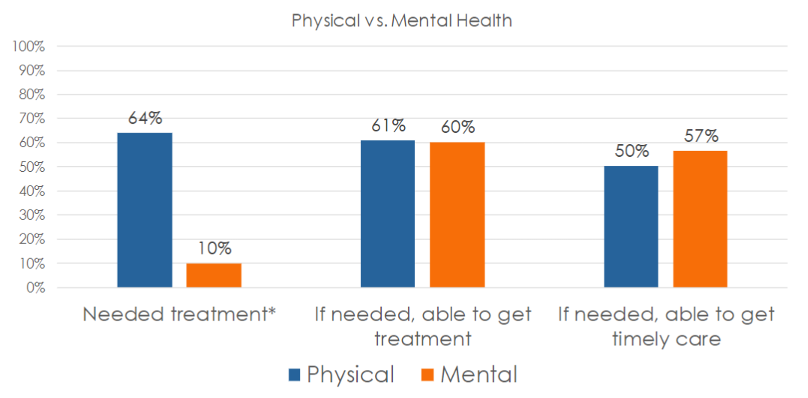
In its Accelerating Integrated Care webinar series , the Pacific Business Group on Health’s (PBGH) California Quality Collaborative presented results from the most recent PBGH Patient Assessment Survey (PAS). The research measured the experience of 35,000 Californians regarding mental health screening and access to necessary treatment. Also measured was the degree to which patients were successful getting timely access to physical versus mental health care.
Screening Rates and Access to Mental Health Treatment are Low
Participants of the survey visited either a primary care or specialty medical provider between July and October of 2019 and were asked to rate their experiences with their medical care during the six months prior to receiving the survey. Survey participants were asked a series of questions, including:
- Were you asked about mental health symptoms during your medical visit during the past six months?
- Was treatment recommended?
- Did you need treatment?
- Were you able to get care?
- Were you able to get care when you needed it?
Many patients (67%) said that no one from their provider’s office – whether a primary care or specialist visit — had asked them about their mental health, despite 16% reporting feeling they needed care and 30% having accessed care on their own. One-third (33%) said a provider asked them about their mental health.
Half of all patients who were screened were recommended for mental health treatment. Two-thirds agreed they needed the care that was recommended.

Whether in need of mental or physical health care, 60% of those surveyed said they were always able to get access to needed services. Surprisingly, a higher percentage of survey participants in need of mental health services (57%) said they were able to get care when they needed it, compared to just 50% seeking physical health services.
Using Patient Reported Data to Improve Access to Mental Health Care
All provider organizations can utilize this data to improve upon the rate at which patients are screened for mental health symptoms and to ensure they gain access to needed care. Using either baseline data or the Patient Assessment Survey data presented here as a proxy, comparisons against state benchmarks to set goals for screening and access can be made. To begin improvement work, select evidence-based change tactics to create an action plan.
It is important to ask patients about their experiences accessing care at your organization. Encounter and claims data can be useful in instances when patients who have been seen for a medical appointment have also filled out a screening tool, though this data do not capture whether the patient was satisfied with their experience and felt they received care when they needed it. Follow the steps below to capture feedback from patients to identify populations that might need extra support.
If your organization does not already collect such data:
- Measure: Develop a survey to collect patient data.
- Interpret: Use the data presented in this article as a proxy benchmark until you collect your own data – assume your screening and access rates are similar (33% screened, 60% able to access care).
If your organization already collects patient experience data for mental health care:
- Measure: Identify a contact at your organization who can provide data on mental health screening and access.
- Interpret: Compare your internal data to the statewide data presented in this webinar (33% screened, 60% able to access care) – how does your organization compare? Which populations might need extra support?
For more details on upcoming CQC webinars focusing on how to improve mental health screenings and access to mental health treatment in primary care settings, sign up for the CQC Newsletter or visit the Webinars webpage . Later this year, PBGH will publish an Issue Brief with further results from this study. For more information, find the full recording of this webinar here and the slide deck here.