Purchaser Innovation and Policy Engagement Against a Backdrop of Unaffordability and Fiduciary Risk
March 31st, 2025
Tags:
Behavioral Health,
CAA,
cost containment,
fiduciary,
health policy,
healthcare costs,
healthcare value,
HPT,
Primary Care,
procurement,
TiCThe U.S. is confronting a health care affordability crisis. Health care cost increases have exceeded general inflation for decades and the gap has widened in recent years, with 2025 on track for health care spending to grow at its highest level in 13 years. The high and rising cost of health care – resulting primarily from high prices fueled by consolidation – is unsustainable.
Public and private purchasers who make up a significant portion of the commercial market are financially responsible for the majority of employee health care costs. As costs have soared, spending on health care has crowded out wages, dampened job growth, reduced business investment, and threatened state and local budgets.
Against this backdrop, purchasers are innovating on several fronts and taking new approaches to multiple health care strategies. They are purchasing care differently, choosing partners wisely, using transparent data to make more informed decisions, and scrutinizing their health plan for value. At the same time, purchasers recognize that the need to directly engage in state and federal health policy to support their strategies has never been more important.
Read our full issue brief on how large purchasers are meeting the moment by contending with the affordability crisis through innovations to how they procure and manage health care and advocate for pro-competitive health care policy reforms.
How Primary Care Providers Can Improve Depression Screening
May 4th, 2021
Depression screening is an essential tool for primary care providers to better understand and meet their patients’ needs, especially as behavioral health conditions have dramatically increased in the past year. Patient-centric approaches and thoughtful implementation of depression screening can lead to earlier intervention, improved overall health outcomes and reduced utilization of health care services.
In March 2021, PBGH’s California Quality Collaborative (CQC) hosted a webinar on the importance of depression screening for patients, providers and payers and shared practical advice for patient-centered depression screening. Experts from PBGH, Montefiore Medical Center and UCLA identified four key takeaways during the discussion:
1. Primary care providers should start screening patients for depression now. There is increasing demand being placed on primary care clinicians to screen patients for depression. Health plans, employers and other purchasers of health care recognize that depression affects millions of patients, and they are investing in behavioral health as a strategy to improve health outcomes. In California, there is momentum from organizations like the Integrated Healthcare Association, which runs statewide performance improvement programs, and Covered California, to include depression screening as a required health care quality measure. Providers will be financially accountable for completing depression screening in the next several years as part of existing pay-for-performance programs.
2. Care teams need training to be comfortable screening patients for depression. Care teams require resources and information about depression screening and how to follow up appropriately with patients in need of behavioral health services. Specialized trainings with role-playing opportunities are effective, as are resources, such as a list of frequently asked questions developed by the Advancing Integrated Mental Health Solution (AIMS) Center from University of Washington.
3. Screening workflows can be integrated into virtual visits, with intentional planning. During the public health emergency, UCLA Health increased the use of virtual primary care visits. The system’s clinical and operations teams created a depression screening workflow that leveraged “virtual rooming” steps, during which clinical support staff register and prepare patients for telehealth visits just as they would for in-person clinical appointments. To address safety concerns associated with suicidal ideation documented in patient depression questionnaires, they tested and implemented several solutions by which the provider would monitor a patient’s response, or the electronic health record would issue an automatic alert.
4. Technology can expand the reach of primary care to provide whole-person care. Montefiore Medical Center launched a smartphone app that includes screening, educational resources, appointment and medication reminders and near real-time chat, among other features. Providers using the Montefiore app with their patients found that it improved behavioral health care engagement with a diverse set of patient populations. In an analysis of the smartphone app pilot data, 72% of patients used it to access educational articles and videos, 69% used it to interact with their care teams via secure chat or text and 67% used the app to complete a depression or other behavioral screening scale.
For additional insights about how primary care providers can improve depression screening for their patients, watch the March 31 CQC webinar or access the presentation.
The Current State of Mental Health Screening and Access in California: Results from 35,000 Patients
October 26th, 2020
Mental health concerns are increasingly common, yet many patients in California are not screened for symptoms and are unable to access treatment. Understanding patients’ access to care is challenging; data are scarce and usually only available at a statewide level, even though there are likely wide regional differences due to workforce shortages.
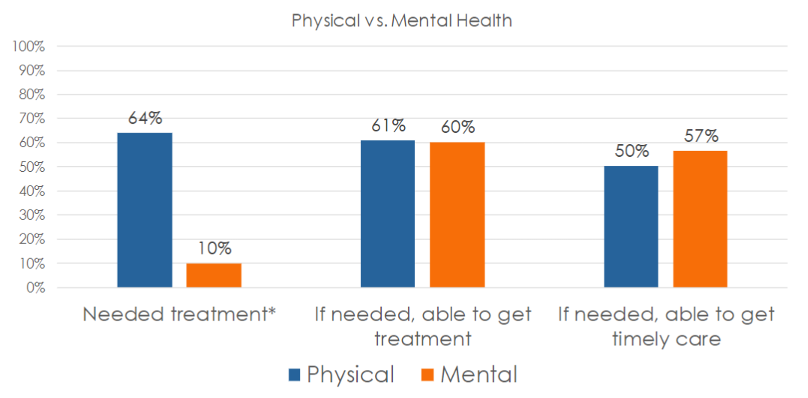
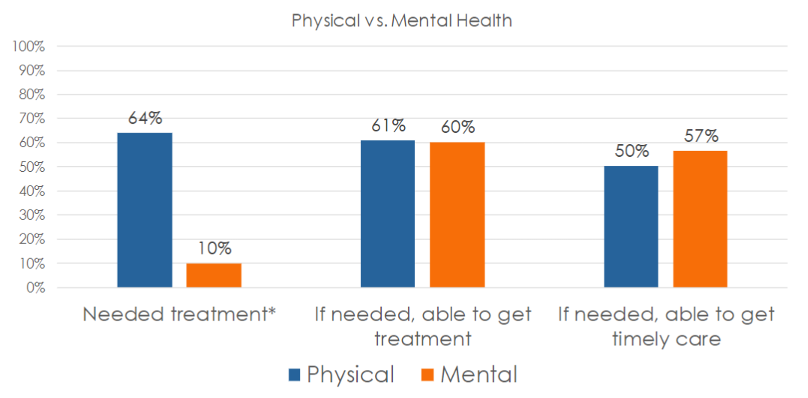
In its Accelerating Integrated Care webinar series , the Pacific Business Group on Health’s (PBGH) California Quality Collaborative presented results from the most recent PBGH Patient Assessment Survey (PAS). The research measured the experience of 35,000 Californians regarding mental health screening and access to necessary treatment. Also measured was the degree to which patients were successful getting timely access to physical versus mental health care.
Screening Rates and Access to Mental Health Treatment are Low
Participants of the survey visited either a primary care or specialty medical provider between July and October of 2019 and were asked to rate their experiences with their medical care during the six months prior to receiving the survey. Survey participants were asked a series of questions, including:
- Were you asked about mental health symptoms during your medical visit during the past six months?
- Was treatment recommended?
- Did you need treatment?
- Were you able to get care?
- Were you able to get care when you needed it?
Many patients (67%) said that no one from their provider’s office – whether a primary care or specialist visit — had asked them about their mental health, despite 16% reporting feeling they needed care and 30% having accessed care on their own. One-third (33%) said a provider asked them about their mental health.
Half of all patients who were screened were recommended for mental health treatment. Two-thirds agreed they needed the care that was recommended.

Whether in need of mental or physical health care, 60% of those surveyed said they were always able to get access to needed services. Surprisingly, a higher percentage of survey participants in need of mental health services (57%) said they were able to get care when they needed it, compared to just 50% seeking physical health services.
Using Patient Reported Data to Improve Access to Mental Health Care
All provider organizations can utilize this data to improve upon the rate at which patients are screened for mental health symptoms and to ensure they gain access to needed care. Using either baseline data or the Patient Assessment Survey data presented here as a proxy, comparisons against state benchmarks to set goals for screening and access can be made. To begin improvement work, select evidence-based change tactics to create an action plan.
It is important to ask patients about their experiences accessing care at your organization. Encounter and claims data can be useful in instances when patients who have been seen for a medical appointment have also filled out a screening tool, though this data do not capture whether the patient was satisfied with their experience and felt they received care when they needed it. Follow the steps below to capture feedback from patients to identify populations that might need extra support.
If your organization does not already collect such data:
- Measure: Develop a survey to collect patient data.
- Interpret: Use the data presented in this article as a proxy benchmark until you collect your own data – assume your screening and access rates are similar (33% screened, 60% able to access care).
If your organization already collects patient experience data for mental health care:
- Measure: Identify a contact at your organization who can provide data on mental health screening and access.
- Interpret: Compare your internal data to the statewide data presented in this webinar (33% screened, 60% able to access care) – how does your organization compare? Which populations might need extra support?
For more details on upcoming CQC webinars focusing on how to improve mental health screenings and access to mental health treatment in primary care settings, sign up for the CQC Newsletter or visit the Webinars webpage . Later this year, PBGH will publish an Issue Brief with further results from this study. For more information, find the full recording of this webinar here and the slide deck here.
Supporting Employee Mental Health During COVID: 4 Best Practices for Employers Considering Digital Solutions
September 8th, 2020
The COVID pandemic has created a rise of mental health concerns. One in four people already struggle with their mental health, and recent reports indicate 45% of people feel their mental health has been worsened by the pandemic. Mental health conditions are greatly impacting the workforce, with wide-reaching implications for well-being and workplace productivity.
Treatment can greatly reduce mental health symptoms, but many patients are not receiving proper care. Up to 60% do not receive treatment, and people often suffer for 10 years or more before receiving care. Access, cost and stigma pose significant barriers to the successful treatment of mental health disorders.
Digital is Trying to Fill the Gap
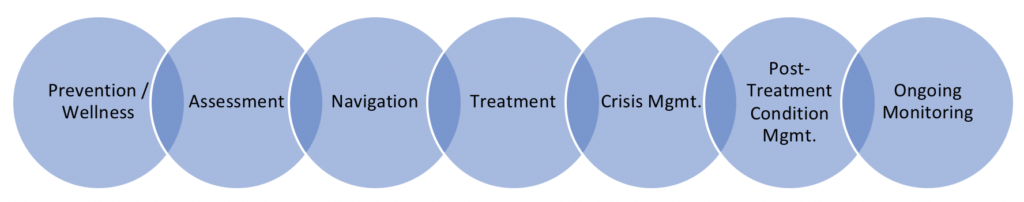
Digital tools have promised to alleviate many of the pain points with traditional mental health care.With 88% of Americans owning a smartphone, general interest in digital health care solutions has surged, as have the options for tapping into care via smartphone or other digital devises. There are as many as an estimated 22,000 digital mental health apps available to consumers offering care that spans from prevention to treatment.
Uses for Digital Mental Health Care
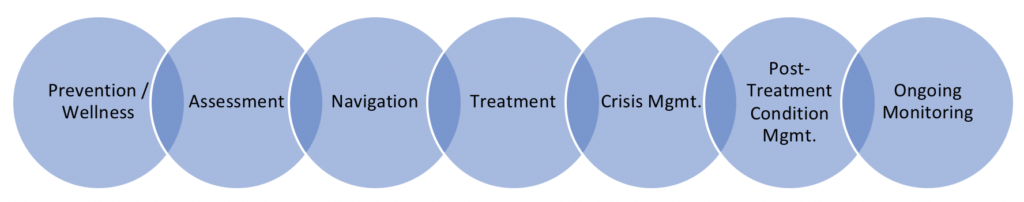
Large employers have an increasing interest in using digital tools to increase access for employees to behavioral and mental health benefits. While employer adoption of apps is currently low (not topping 11% of employers), more than 30% of employers plan to offer these services in the next few years. Recently conducted research with 10 large employers highlights their desire for on-demand access to a carefully selected network of providers, the ability to connect employees with a human, care based on evidence and that the user experience will be good.
4 Best Practices When Selecting Digital Tools
Select Carefully
- Analyze your claims data to understand your top conditions and how much your company is spending on behavioral and mental health services
- Select tools that are specific to the top needs identified in your claims data analysis (i.e., if your top spend is on depression, select a tool that is designed to address depression)
- Gather referrals from other employers (an employer coalition is a great way to connect with peers
- Ask your benefits team to test the product themselves for ease of use, customer service and content quality; select tools that are highly rated by the team.
Make Offerings Easy to Find and Access
- Consider a single sign-on (SSO) for all benefits so employees can easily find the tool
- Reduce the number of sign-ons required for users to access the tool
- Encourage employees to create accounts before they need to access services – consider a benefits sign-up pledge to increase adoption
Develop an Employee Communications Strategy
- Create a communication campaign around employee mental health that includes information on available employee resources, information on mental health conditions and tips to improve emotional wellness
- Consider using an employee resource group to review campaign messaging before it is distributed to avoid stigmatizing terms
- Ask if employees are interested in forming volunteer employee resource groups around mental health
- Identify leadership champions and have open communication around mental health
- Increase communications during mental health awareness monthUse the vendor to help design an engagement plan to promote use of the tool – it’s their job!
Ongoing Evaluation of the plan is Essential
- Monitor employee engagement with your communications – track website clicks, tool downloads and webinar attendance to identify popular topics and increase offerings based on positive employee feedback
- Gather employee feedback through focus groups
- Set success metrics upfront, and have patience (within reason)
- Request frequent vendor data on outcomes, utilization, retention, user satisfaction
- Plug the gaps – regularly re-assess your employee needs, if your solutions are meeting those needs, and modify solutions accordingly.
The digitalization of health care is expected to increase exponentially in the next few years, catapulted by COVID-19. The pandemic has landed a one-two punch; in-person care has been limited and an increase of mental health issues is expected. Our current delivery system is not set up to care for people with mental health needs, especially those with lower incomes who cannot afford to pay cash for out-of-network care. Digital tools may play an important role in bridging that divide. Be sure to follow the 4 success factors above to increase your chances of success.
To read more about digital mental health tools used in the workplace, see Digital Solutions for Employee Mental Health.
The Silent Pandemic of Loneliness
May 7th, 2020
Already pervasive in the modern world, loneliness and social isolation are extending their reach deeper into the American workforce as the COVID-19 pandemic upends the routines and relationships of daily life. The physical distancing required to manage COVID-19 should not be confused with social distancing and isolation.
Helping employees overcome feelings of isolation is more important now than ever, given the serious physical and psychological effects that extended bouts of loneliness can produce, according to a presenter at a recent webinar sponsored by the Pacific Business Group on Health.
Jeremy Nobel, M.D., a primary care physician and faculty member at the Harvard T.H. Chan School of Public Health, laid out the business case for reducing workplace loneliness. Nobel spearheads The UnLonely Project, a signature initiative of the non-profit Foundation for Art & Healing, designed to broaden public awareness about the negative health consequences of loneliness while promoting creative arts-based approaches for reducing the burden of isolation.
The Toll of Loneliness
Loneliness—defined as the subjective discrepancy between desired and actual social relations—had already reached epidemic levels in the U.S. before the onset of COVID-19, according to Nobel. A January survey found that 79% of people who are part of Generation Z, 71% of millennials and 50% of baby boomers feel lonely.
Nobel said loneliness is especially prevalent among individuals under significant stress or facing difficult life circumstances, such as chronic illness, disability or the loss of a loved one. Those who may be particularly vulnerable include minorities, veterans, LGBTQ employees, caregivers, pre-retiree workers and anyone with a major or chronic physical or mental illness condition. Specific age groups, notably adolescents, young adults and older adults, appear at higher risk as marked by growing incidence of depression, substance abuse and suicide.
The health impacts of loneliness are significant:
- Evidence indicates substantial negative effects on mental health, including worsening depression, anxiety and cognitive decline.
- Loneliness is more likely to result in higher rates of cardiovascular illness, chronic pain and fatigue. Research suggests the long-term physical harm of loneliness is not unlike the health effects of obesity or smoking, increasing the risk of mortality by up to 30%.
In the workplace, loneliness drives up the cost of care and also affects employee performance, morale and retention, according to Nobel. It contributes to stress and burnout and can reduce workers’ ability to collaborate effectively and engage with customers and co-workers. Further, loneliness undermines the development of a culture of inclusion and belonging.
New concerns have emerged with the pandemic, including increased risk for depression, suicide and addiction; productivity and performance declines; and greater risks of abandonment of self-care for pre-existing chronic conditions.
Employer Strategies
Nobel pointed to several strategies employers can pursue to help employees mitigate feelings of loneliness. These include:
- Education: Communicate the physical and mental risks related to isolation and loneliness, and clarify the relationship between stress, burnout and social isolation – both at home and in the workplace
- Engagement: Build on existing employee assistance programs (EAP) with additional activities designed to promote engagement and connection, including initiatives that specifically address mindfulness and purpose; emphasize stress management and resilience skill-building
- Access: Make it easy for people to ask for help, expand mental first-aid training and explore peer-to-peer support programs
- Measurement: Think of mental health as a vital sign. Screen for loneliness risk using employee surveys, performance indicators and claims, and be sensitive to early, mid-stage and advanced levels of impairment
Because engaging in creative activities can have a positive effect on both mental and physical health, organizations should also explore opportunities for promoting the development of creative outlets.
To learn more about the role of creativity in improving health, visit The UnLonely Project and a companion initiative, Stuck at Home (together).