Behavioral Health Integration Initiative
Meeting patients’ mental health needs and considering social impacts on their health are fundamental to providing comprehensive, patient-centered and high-quality care. However, the lack of improvement in screening and care access demonstrates the need for greater investment to support primary care practices in efforts to integrate behavioral health services.
CQC will work on a Behavioral Health Integration Initiative from 2022 through 2027 that will accelerate integration efforts by small and independent primary care practices throughout the state. The initiative aims to improve screening, diagnosis and treatment of patients’ mild-to-moderate behavioral health needs, like depression, anxiety and substance use disorder.
This includes:
- Direct technical assistance and funding to primary care practices engaged in improvement efforts through the CalHIVE Behavioral Health Integration Improvement Collaborative
- Better understanding patient perspectives of their behavioral health needs, access to care and treatment through expanded surveying
- Development of common standards for patient privacy, consent and data sharing among payers and providers to reduce administrative burden to integrating care
Support
CQC’s Behavioral Health Integration Initiative is possible thanks to the generous support of Centene Corporation, California Health Care Foundation and Blue Shield California Industry Initiatives.
Programs
CalHIVE Behavioral Health Integration (2023-2026)
Read More about CalHIVE Behavioral Health Integration (2023-2026)The CalHIVE Behavioral Health Integration Improvement Collaborative is a three-year program operated by PBGH’s California Quality Collaborative (CQC) that begins July 2023 and will focus on supporting California-based primary care practices as they integrate behavioral health services.
Behavioral Health Integration – Children and Youth Collaborative Learning Exchange (2024-2025)
Read More about Behavioral Health Integration – Children and Youth Collaborative Learning Exchange (2024-2025)The Behavioral Health Integration – Children and Youth Collaborative Learning Exchange is a nine-month learning collaborative launching October 2024 that will bring together organizations experienced in integrating behavioral health services into primary care for children and youth.
Collective BHI Solutions – Behavioral Health Integration Financing (2024)
Read More about Collective BHI Solutions – Behavioral Health Integration Financing (2024)Through Behavioral Health Integration Financing, CQC will conduct a state-wide landscape assessment project to identify, synthesize and communicate successful practices to ensure sustainable payment for behavioral health integration into primary care.
Cal-IN Peer Group (2024)
Read More about Cal-IN Peer Group (2024)CQC is hosting quarterly peer group meetings for individuals working to integrate behavioral health care into the primary care setting in California.
Resources

Behavioral Health Integration Billing and Coding Sheet

BHI Quarterly Implementation Update

Behavioral Health Integration Initiative Annual Report Annual Report 2023

BHI Snapshot | Selecting an Integration Model

Behavioral Health Integration Implementation Plan
Our BHI Implementation Plan guides organizations through the creation of a plan that integrates multi-disciplinary team feedback to determine the integration model that best meets organizational needs.

Behavioral Health Integration Improvement Collaborative Curriculum
CQC Toolkit: Implement Adverse Childhood Experiences Screening in Primary Care
This toolkit is a collection of evidence-based interventions and resources for ambulatory care provider organizations to implement Adverse Childhood Experiences (ACE) screening and follow-up care.
CIN Toolkit: Three Strategies to Help Primary Care Teams Treat Substance Use Disorders
This document is a guide for primary care organizations and care teams working to integrate substance use disorder (SUD) treatment services.

Accelerating Opioid Safety Ambulatory Care Toolkit
The following document is a guide for provider organizations working to improve opioid safety — to prevent new populations of patients from becoming dependent on or addicted to opioids and improve care for patients with chronic non-cancer pain, opioid use disorder, and/or at risk of overdose.
Upcoming Events and Training

CFHA Integrated Care Conference
Crystal Eubanks, Executive Director at the California Quality Collaborative and Vice President of Care Transformation at the Purchaser Business Group on Health, will present on the California Advanced Primary Care Initiative’s work to improve primary care delivery.

Behavioral Health Integration Implementation Webinar Series
The California Quality Collaborative’s Behavioral Health Integration Implementation Webinar Series is a three-part webinar series for health care organizations planning and implementing behavioral health integration.

Cal-IN Peer Group
In partnership with the Collaborative Family Healthcare Association, the California Quality Collaborative is hosting quarterly virtual peer group meetings for individuals working to integrate behavioral health care into the primary care setting in California.
Past Events and Training

Behavioral Health Integration Financing Convening
The California Quality Collaborative’s Behavioral Health Integration Financing Convening brings together stakeholders to explore findings from statewide interviews on sustainable payment practices and brainstorm improvement opportunities for integrating behavioral health into primary care.

Behavioral Health Integration Financing Convening
The California Quality Collaborative’s Behavioral Health Integration Financing Convening brings together stakeholders to explore findings from statewide interviews on sustainable payment practices and brainstorm improvement opportunities for integrating behavioral health into primary care.

CQC Webinar: Behavioral Health Integration – Children and Youth Collaborative Learning Exchange Program
BHI-CYCLE is a nine-month learning collaborative beginning October 2024 that will bring together organizations experienced in integrating behavioral health services into primary care for children and youth.

2024 CalHIVE Behavioral Health Integration Annual Convening
The California Quality Collaborative’s CalHIVE Behavioral Health Integration Annual Convening is a two-day learning and networking session for improvement collaborative participants.

Behavioral Health Integration Fundamentals: Concepts & Models
Integrating behavioral health into primary care is essential for providers looking to deliver patient-centered, high-quality and whole-person care. Yet many health care organizations struggle with knowing where to begin.

CQC Webinar – Behavioral Health Integration: Telehealth Promising Practices
Hear on-the-ground lessons around behavioral health integration, and understand opportunities around effective virtual care.

CQC Webinar: Increase Adverse Childhood Experiences (ACEs) Screening
Part of our ongoing Accelerated Integrated Care Series, Adverse Childhood Experiences (ACEs) are potentially traumatic events that occur in childhood and have been linked to more than 40 negative health conditions.
CQC Webinar: Increase Depression Screening
In this meeting, attendees shared challenges and questions related to depression screening at their organizations, and identified a next step they could apply at their own organizations.
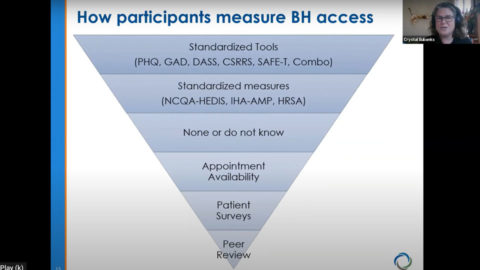
Measure Screening and Access for Behavioral Health
Results from a Patient Assessment Survey (PAS) from a study of 35,000 patients across California were shared and discussion about how organizations can use data to help identify populations that need additional mental health support.