The Current State of Mental Health Screening and Access in California: Results from 35,000 Patients

Mental health concerns are increasingly common, yet many patients in California are not screened for symptoms and are unable to access treatment. Understanding patients’ access to care is challenging; data are scarce and usually only available at a statewide level, even though there are likely wide regional differences due to workforce shortages.
In its Accelerating Integrated Care webinar series , the Pacific Business Group on Health’s (PBGH) California Quality Collaborative presented results from the most recent PBGH Patient Assessment Survey (PAS). The research measured the experience of 35,000 Californians regarding mental health screening and access to necessary treatment. Also measured was the degree to which patients were successful getting timely access to physical versus mental health care.
Screening Rates and Access to Mental Health Treatment are Low
Participants of the survey visited either a primary care or specialty medical provider between July and October of 2019 and were asked to rate their experiences with their medical care during the six months prior to receiving the survey. Survey participants were asked a series of questions, including:
- Were you asked about mental health symptoms during your medical visit during the past six months?
- Was treatment recommended?
- Did you need treatment?
- Were you able to get care?
- Were you able to get care when you needed it?
Many patients (67%) said that no one from their provider’s office – whether a primary care or specialist visit — had asked them about their mental health, despite 16% reporting feeling they needed care and 30% having accessed care on their own. One-third (33%) said a provider asked them about their mental health.
Half of all patients who were screened were recommended for mental health treatment. Two-thirds agreed they needed the care that was recommended.

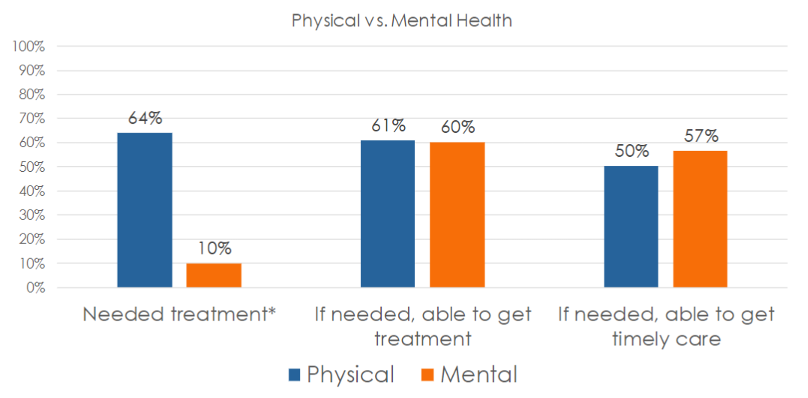
Whether in need of mental or physical health care, 60% of those surveyed said they were always able to get access to needed services. Surprisingly, a higher percentage of survey participants in need of mental health services (57%) said they were able to get care when they needed it, compared to just 50% seeking physical health services.
Using Patient Reported Data to Improve Access to Mental Health Care
All provider organizations can utilize this data to improve upon the rate at which patients are screened for mental health symptoms and to ensure they gain access to needed care. Using either baseline data or the Patient Assessment Survey data presented here as a proxy, comparisons against state benchmarks to set goals for screening and access can be made. To begin improvement work, select evidence-based change tactics to create an action plan.
It is important to ask patients about their experiences accessing care at your organization. Encounter and claims data can be useful in instances when patients who have been seen for a medical appointment have also filled out a screening tool, though this data do not capture whether the patient was satisfied with their experience and felt they received care when they needed it. Follow the steps below to capture feedback from patients to identify populations that might need extra support.
If your organization does not already collect such data:
- Measure: Develop a survey to collect patient data.
- Interpret: Use the data presented in this article as a proxy benchmark until you collect your own data – assume your screening and access rates are similar (33% screened, 60% able to access care).
If your organization already collects patient experience data for mental health care:
- Measure: Identify a contact at your organization who can provide data on mental health screening and access.
- Interpret: Compare your internal data to the statewide data presented in this webinar (33% screened, 60% able to access care) – how does your organization compare? Which populations might need extra support?
For more details on upcoming CQC webinars focusing on how to improve mental health screenings and access to mental health treatment in primary care settings, sign up for the CQC Newsletter or visit the Webinars webpage . Later this year, PBGH will publish an Issue Brief with further results from this study. For more information, find the full recording of this webinar here and the slide deck here.



