Supporting Employee Mental Health During COVID: 4 Best Practices for Employers Considering Digital Solutions

The COVID pandemic has created a rise of mental health concerns. One in four people already struggle with their mental health, and recent reports indicate 45% of people feel their mental health has been worsened by the pandemic. Mental health conditions are greatly impacting the workforce, with wide-reaching implications for well-being and workplace productivity.
Treatment can greatly reduce mental health symptoms, but many patients are not receiving proper care. Up to 60% do not receive treatment, and people often suffer for 10 years or more before receiving care. Access, cost and stigma pose significant barriers to the successful treatment of mental health disorders.
Digital is Trying to Fill the Gap
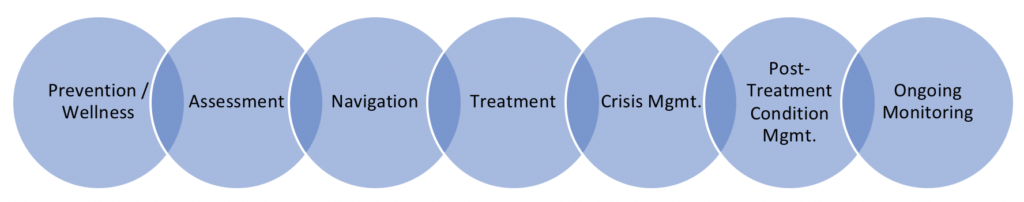
Digital tools have promised to alleviate many of the pain points with traditional mental health care.With 88% of Americans owning a smartphone, general interest in digital health care solutions has surged, as have the options for tapping into care via smartphone or other digital devises. There are as many as an estimated 22,000 digital mental health apps available to consumers offering care that spans from prevention to treatment.
Uses for Digital Mental Health Care
Large employers have an increasing interest in using digital tools to increase access for employees to behavioral and mental health benefits. While employer adoption of apps is currently low (not topping 11% of employers), more than 30% of employers plan to offer these services in the next few years. Recently conducted research with 10 large employers highlights their desire for on-demand access to a carefully selected network of providers, the ability to connect employees with a human, care based on evidence and that the user experience will be good.
4 Best Practices When Selecting Digital Tools
Select Carefully
- Analyze your claims data to understand your top conditions and how much your company is spending on behavioral and mental health services
- Select tools that are specific to the top needs identified in your claims data analysis (i.e., if your top spend is on depression, select a tool that is designed to address depression)
- Gather referrals from other employers (an employer coalition is a great way to connect with peers
- Ask your benefits team to test the product themselves for ease of use, customer service and content quality; select tools that are highly rated by the team.
Make Offerings Easy to Find and Access
- Consider a single sign-on (SSO) for all benefits so employees can easily find the tool
- Reduce the number of sign-ons required for users to access the tool
- Encourage employees to create accounts before they need to access services – consider a benefits sign-up pledge to increase adoption
Develop an Employee Communications Strategy
- Create a communication campaign around employee mental health that includes information on available employee resources, information on mental health conditions and tips to improve emotional wellness
- Consider using an employee resource group to review campaign messaging before it is distributed to avoid stigmatizing terms
- Ask if employees are interested in forming volunteer employee resource groups around mental health
- Identify leadership champions and have open communication around mental health
- Increase communications during mental health awareness monthUse the vendor to help design an engagement plan to promote use of the tool – it’s their job!
Ongoing Evaluation of the plan is Essential
- Monitor employee engagement with your communications – track website clicks, tool downloads and webinar attendance to identify popular topics and increase offerings based on positive employee feedback
- Gather employee feedback through focus groups
- Set success metrics upfront, and have patience (within reason)
- Request frequent vendor data on outcomes, utilization, retention, user satisfaction
- Plug the gaps – regularly re-assess your employee needs, if your solutions are meeting those needs, and modify solutions accordingly.
The digitalization of health care is expected to increase exponentially in the next few years, catapulted by COVID-19. The pandemic has landed a one-two punch; in-person care has been limited and an increase of mental health issues is expected. Our current delivery system is not set up to care for people with mental health needs, especially those with lower incomes who cannot afford to pay cash for out-of-network care. Digital tools may play an important role in bridging that divide. Be sure to follow the 4 success factors above to increase your chances of success.
To read more about digital mental health tools used in the workplace, see Digital Solutions for Employee Mental Health.



